Contents
Abstract
Functioning as the exterior interface of the human body with the environment, skin acts as a physical barrier to prevent the invasion of foreign pathogens while providing a home to the commensal microbiota. The harsh physical landscape of skin, particularly the desiccated, nutrient-poor, acidic environment, also contributes to the adversity that pathogens face when colonizing human skin. Despite this, the skin is colonized by a diverse microbiota. In this Review, we describe amplicon and shotgun metagenomic DNA sequencing studies that have been used to assess the taxonomic diversity of microorganisms that are associated with skin from the kingdom to the strain level. We discuss recent insights into skin microbial communities, including their composition in health and disease, the dynamics between species and interactions with the immune system, with a focus on Propionibacterium acnes, Staphylococcus epidermidis and Staphylococcus aureus.
Introduction
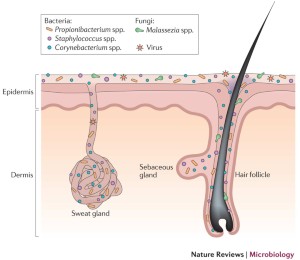
Our skin is home to millions of bacteria, fungi and viruses that compose the skin microbiota. Similar to those in our gut, skin microorganisms have essential roles in the protection against invading pathogens, the education of our immune system and the breakdown of natural products1,2,3. As the largest organ of the human body, skin is colonized by beneficial microorganisms and serves as a physical barrier to prevent the invasion of pathogens. In circumstances where the barrier is broken or when the balance between commensals and pathogens is disturbed, skin disease or even systemic disease can result. Human skin sites can be categorized by their physiological characteristics, that is, whether they are sebaceous (oily), moist or dry (Box 1). Studying the composition of the microbiota at different sites is valuable for elucidating the aetiology of common skin disorders, which often have a preference for specific skin sites, such as eczema inside the elbow4 and psoriasis on the outside of the elbow5.
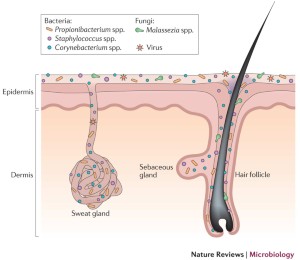
Traditionally, skin microbial communities were explored by use of culture-based methods. As this approach selects for microorganisms that thrive in artificial growth conditions, it underestimates the total diversity of the community. For example, the skin genus Staphylococcus is cultivated more easily than Propionibacterium spp. or Corynebacterium spp., which were frequently underestimated in culture-based surveys6. Thus, to circumvent the bias imposed by culture and to capture the complete diversity of the microbiome, investigators began applying sequencing methods. These original sequencing approaches utilized sequence variation in conserved taxonomic markers as molecular fingerprints to identify members of microbial communities7. For bacteria, the 16S ribosomal RNA (rRNA) gene is used, whereas for fungi, the internal transcribed spacer 1 (ITS1) region of the eukaryotic ribosomal gene is preferred8.
As sequencing technologies have advanced from Sanger sequencing to 454 pyrosequencing and then Illumina sequencing, this original approach has been regularly adapted to accommodate increasing read depths and shorter read lengths. This has been accomplished with new primers for shorter amplicons, clustering methods to overcome sequencing error and assembly methods to combine paired-end reads. With shorter amplicon lengths (∼300 bp compared with >1,000 bp in Sanger sequencing), only a subregion of the 16S rRNA gene can be analysed. This requires optimized primers that bind to specific regions of the 16S rRNA gene to capture the genetic diversity of the bacterial population; primer pairs that are used in skin microbiome studies should be optimized to amplify and distinguish prevalent cutaneous microbial taxa9,10,11. To date, the primary pipelines for analysing amplicon data are mothur12 and Qiime13. Both methods use a read clustering approach by which clustered reads are compared with curated reference databases to classify communities at the genus and, when possible, the species level.
Most skin microbiome surveys have used amplicon sequencing. Over the past few years, however, major technical and analytical breakthroughs have enabled shotgun metagenomic sequencing studies. Figure 1 highlights the technical and procedural differences between amplicon and shotgun metagenomics and the different types of analyses that are possible with the data sets. As shotgun metagenomics does not sequence specific target regions, it simultaneously captures all genetic material in a sample, including human, bacterial, fungal, archaeal and viral, thus allowing relative kingdom abundances to be inferred, with the limitation that the DNA of different microorganisms may be differentially extracted depending on the sample preparation method14,15,16. Another advantage of shotgun metagenomic sequencing is that these data sets provide sufficient resolution to differentiate species and even strains within a species. This is crucial for identifying members of the Staphylococcus genus, which are difficult to classify to the species level with most amplicon sequencing approaches9. The ability to differentiate strains is important as more studies reveal the functional differences that exist between strains within a species17,18,19.
To study the members of a microbial community, two sequencing strategies can be utilized. For amplicon sequencing (left), primers are utilized that amplify conserved regions within a kingdom. For bacteria, the 16S ribosomal RNA (rRNA) region of the ribosomal gene is amplified, whereas for fungi, the internal transcribed spacer 1 (ITS1) region is amplified. By contrast, whole genome sequencing (right) captures the entire complement of genetic material in a sample without a targeted amplification step. Analyses of sequenced amplicons can identify the genus-level and the species-level community composition, but only shotgun metagenomics can reveal kingdom relative abundances and resolution to the strain level. Colours not defined may be grouped as ‘Other’.
In this Review, we discuss recent insights into skin microbial communities, including their composition in health and disease, assembly and ecology, and interactions with the immune system. We end by considering important unanswered questions in the field and future research priorities. A greater understanding of these topics is important as interest in targeting the skin microbiome for therapeutic approaches increases.
The skin microbiota in health
Before investigating changes in the microbiota that are associated with a disease state, scientists must first establish a baseline and the normal variation in the microbiota of healthy individuals.
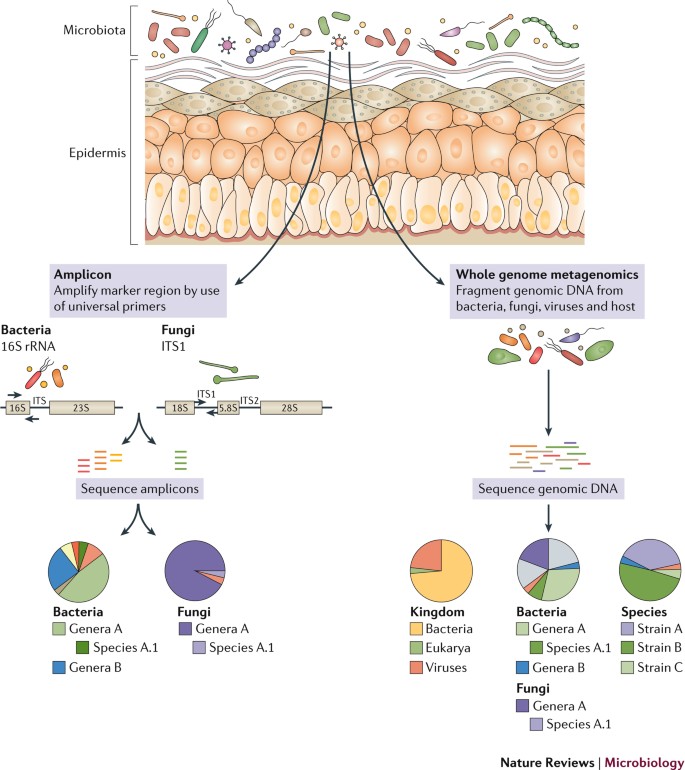
Composition of the skin microbiota. In sequencing surveys of healthy adults20,21,22,23, the composition of microbial communities was found to be primarily dependent on the physiology of the skin site, with changes in the relative abundance of bacterial taxa associated with moist, dry and sebaceous microenvironments. Sebaceous sites were dominated by lipophilic Propionibacterium species, whereas bacteria that thrive in humid environments, such as Staphylococcus and Corynebacterium species, were preferentially abundant in moist areas, including the bends of the elbows and the feet (Fig. 2; Table 1). In contrast to bacterial communities, fungal community composition was similar across core body sites regardless of physiology23,24. Fungi of the genus Malassezia predominated at core body and arm sites, whereas foot sites were colonized by a more diverse combination of Malassezia spp., Aspergillus spp., Cryptococcus spp., Rhodotorula spp., Epicoccum spp. and others24 (Fig. 2). Bacteria were the most abundant kingdom across sites, and fungi were the least abundant25 (Fig. 2); however, there are many more bacterial reference genomes than fungal reference genomes available, which may partially contribute to this observed difference. Interestingly, the overall fungal abundance was low, even on the feet where fungal diversity was high.
Four sites are shown to represent major microenvironments of the skin: glabella (also known as the forehead) sebaceous (oily); antecubital fossa (moist); volar forearm (dry); and toe web space (foot). Pie charts represent consensus relative abundances of the kingdom, fungi and bacteria across healthy adults2. The bacterial species Propionibacterium acnes and Staphylococcus epidermidis and eukaryotic DNA viruses are displayed as bar charts for four representative individuals to highlight how individuality shapes these communities25. For kingdom, fungi, bacteria and virus relative abundance plots, major taxa colours are identified in the legend. Unlabelled colours may be grouped as ‘Other’. For the P. acnes and S. epidermidis bar charts, similar colours represent closely related strains.
In contrast to bacteria and fungi, colonization by eukaryotic DNA viruses was specific to the individual rather than anatomical site25 (Fig. 2). As no marker gene is universally shared among viruses, viral community diversity can be captured only with purified viral-like particles or shotgun metagenomics sequencing25,26. As an additional challenge, RNA viruses can be sequenced only with RNA sequencing, which has not been performed on skin samples from healthy individuals. Apart from bacteriophages, particularly those associated with Propionibacterium spp. and Staphylococcus spp., no core DNA virome has been found to be conserved across individuals25,26. This area of skin microbiome research requires further attention to understand the role of possible predator–prey or cooperative interactions between bacteriophages and bacteria in microbial community assembly. In addition to bacteriophages, eukaryotic viruses may also have a role in skin diseases, as highlighted by the discovery of Merkel cell polyomavirus, an oncovirus that causes a rare but aggressive form of skin cancer27.
Through the use of longitudinal sampling, skin microbial communities were found to be largely stable over a 2-year study despite constant environmental changes25. Based on analyses at the strain and single-nucleotide level, this stability was determined by the maintenance of strains over time rather than the reacquisition of common species from the environment25. Similarly, in longitudinal surveys of the gut, specific species of an individual’s microbiota have been found to persist for a year28 or more29. Bacterial and fungal communities at sebaceous sites were the most stable. Microbial communities of foot sites were the least stable, and eukaryotic DNA viruses varied the most over time25,26. The relative instability of foot microbial communities might be attributable to the transient presence of fungi in the environment.
Beyond the species level, shotgun metagenomic data provide sufficient resolution to explore strain diversity of dominant skin bacterial species. Compared with the gut, skin has a low microbial biomass that leads to high host and low microbial sequencing depths in metagenomics samples. Despite low read depths, strain identification of prevalent skin species is possible because collections of sequenced reference genomes exist that span the diversity of a species17,18. Across body sites, individuals were found to be colonized by different multi-phyletic communities of Propionibacterium acnes and Staphylococcus epidermidis strains23 (Fig. 2). In addition, S. epidermidis strains from a commensal clade demonstrated site specificity with a tropism for human feet. Describing communities at strain-level resolution is important when the gene content differences between strains within a species can determine functional differences in health and disease. For example, antibiotic resistance and virulence genes are variably present in P. acnes and S. epidermidis strains17,18. Analysis of strain communities of other skin microbiota species will require the creation of additional comprehensive reference genome libraries or the development of new computational tools that are capable of classifying strains from low coverage metagenomic data. Currently, resolution at the strain level without mapping to reference genomes has been limited to single-molecule, long-read metagenomic sequencing studies30. Future functional studies will allow researchers to elucidate whether some strains provide colonization resistance against other strains of the same or different species as an important step in the development of prebiotic and probiotic strategies.
Compared with the richer environment of our intestines, skin lacks many nutrients beyond basic proteins and lipids. To survive in such a cool, acidic and desiccated environment (Box 1), the resident microbiota of our skin have adapted to utilize the resources that are present in sweat, sebum and the stratum corneum1 (Table 1). For example, the facultative anaerobe P. acnes is able to thrive in the anoxic sebaceous gland by using proteases to liberate the amino acid arginine from skin proteins31 and lipases to degrade triglyceride lipids in sebum32; this releases free fatty acids, which promote bacterial adherence33,34,35. In facial samples, sebum levels of the cheek were shown to positively correlate with Propionibacterium spp. abundance36. Interestingly, for mammals such as mice, rats and dogs, which produce smaller quantities of triglyceride-rich sebum, P. acnes grows less well and is thus found at lower abundances37.
The lipids of sebum and the stratum corneum are also utilized by auxotrophic Malassezia and Corynebacterium species, as they are unable to produce their own lipids1. Corynebacterium spp. utilize these lipid compounds to generate the corynemycolic acids that coat their cell surface1. Consistent with the carbohydrate-deficient, lipid-rich environment of the skin, Malassezia spp. genomes are enriched for lipase genes and depleted for carbohydrate-utilizing enzyme genes compared with the genomes of other sequenced fungi38. Such differences may explain why Malassezia species predominate in the adult skin mycobiome. Finally, Staphylococcus spp. have evolved many strategies for surviving on the skin, including the ability to be halotolerant (that is, to withstand the high salt content of sweat) and utilize the urea that is present in sweat as a nitrogen source1. To further promote colonization, various Staphylococcus spp. can also produce adherens that promote attachment to the skin and proteases that liberate nutrients from the stratum corneum1. Overall, the skin harbours a heterogeneous community of microorganisms that each have distinct adaptations to survive on the skin.
Skin microbiota assembly and ecology
Adults stably maintain the composition of their skin microbial communities as assessed for at least 2 years25; however, the forces that shape and maintain these complex communities remain poorly understood.
Initial colonization and population shifts. In newborn babies, initial colonization of the skin is dependent on delivery mode; neonates born vaginally acquire bacteria that colonize the vagina, whereas neonates born via Caesarian section acquire microorganisms that are associated with the skin39,40. The long-term effects of these initial skin colonization modes in neonates remain unknown, and shotgun metagenomic sequencing and strain-level analyses need to be carried out to address this outstanding issue.
In the gut, microbial communities stabilize around 3 years of age41. Before this stabilization, strains are likely acquired from close contacts and family members42 and are predicted to be maintained throughout life29. By contrast, the relative abundance of skin microbial species is restructured during puberty, a time when increased levels of hormones stimulate the sebaceous glands to produce additional sebum. Thus, the skin of postpubescent individuals favours the expansion of lipophilic microorganisms, such as bacterial Propionibacterium spp. and Corynebacterium spp.43 and fungal Malassezia spp.44,45. By contrast, pre-pubescent children have greater abundances of Firmicutes (Streptococcaceae spp.), Bacteroidetes and Proteobacteria (betaproteobacteria and gammaproteobacteria)43 and a more diverse fungal community44. It remains unclear whether new strains are acquired during puberty or whether the relative abundance of existing strains changes. Overall, these age-related changes in the skin microbiota are interesting, as many skin disorders are associated with age. For example, cases of Staphylococcus-associated atopic dermatitis decline in the majority of children before puberty, whereas Malassezia-associated tinea versicolor is more common in adults than children46,47,48. Further studies are also required to characterize the skin microbiota of elderly individuals as physiology and the predisposition to skin infections change.
Interactions between cutaneous microbial species. Microbial community assembly, stability and function are driven by host factors as well as the interactions between these microorganisms. Microorganisms can act competitively to exclude one another or synergistically for mutual benefits. In the skin, Staphylococcus aureus has been the focus of many colonization resistance studies. S. aureus colonizes the nares of one-third of the population, and its presence is a significant risk factor for subsequent infection49,50. In clinical infections, 80% of S. aureus bloodstream isolates match those identified in the nares of the individual49. Eradication of S. aureus in the nares of a surgical patient substantially reduces his or her susceptibility to invasive infections51.
As S. aureus frequently evolves resistance to antibiotics52 and vaccine development has shown limited efficacy53,54, alternative eradication strategies, particularly those that use commensal microorganisms, are an active area of research55. These competition studies are similar to those that explored how soil microorganisms compete via antibiotic production56. The first microorganisms that were reported to inhibit S. aureus biofilm formation were a subset of S. epidermidis strains that express the serine protease glutamyl endopeptidase (Esp; also known as GluSE)57. It was later found that the S. epidermidis Esp of these strains degrades proteins that are crucial for S. aureus biofilm formation and host epithelial adhesion58; when the protease activity of Esp was combined with the antimicrobial activities of β-defensin, the resultant bactericidal activity was sufficient to kill S. aureus in biofilms (Fig. 3). Interestingly, the vast majority of sequenced S. epidermidis isolates contain the esp (gseA) gene17, but in a former study, only a subset expressed the gseA gene under the conditions tested57. This discrepancy is an important reminder that the possession of a gene does not guarantee constitutive expression.
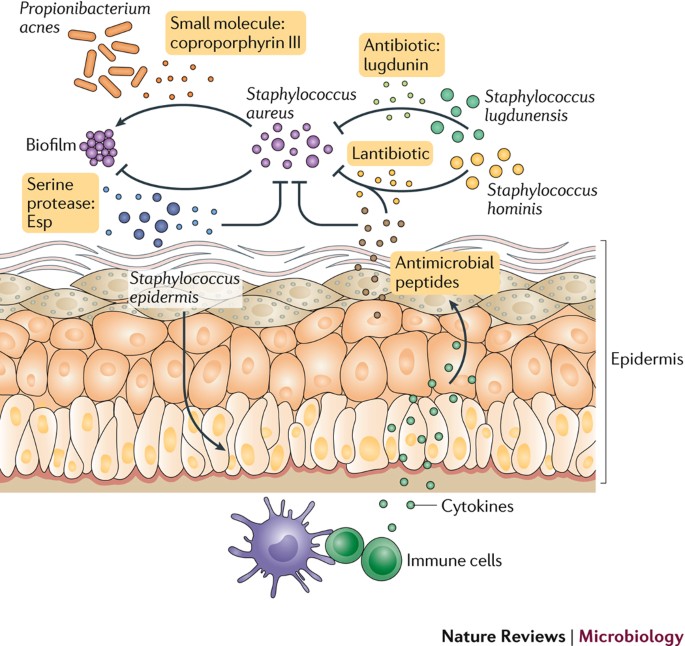
Skin microbial communities are shaped by interactions between organisms and with the host. In the skin, many interactions between commensals and Staphylococcus aureus have been identified. Antibiotics produced by coagulase-negative Staphylococcus and specifically by Staphylococcus lugdunensis prohibit colonization of S. aureus. Also, Staphylococcus epidermidis can inhibit S. aureus biofilm formation with production of the serine protease glutamyl endopeptidase (Esp). Moreover, when Esp-expressing S. epidermidis induces keratinocytes to produce antimicrobial peptides via immune cell signalling, S. aureus is effectively killed. In addition, Staphylococcus hominis-produced lantibiotics synergize with human antimicrobial peptide LL-37 to decrease S. aureus colonization. In contrast to inhibiting S. aureus, Propionibacterium acnes produces a small molecule, coproporphyrin III, that promotes S. aureus aggregation and biofilm formation.
In a more recent study, Staphylococcus lugdunensis inhibited S. aureus growth through the production of the antibiotic lugdunin, a novel thiazolidine-containing cyclic peptide59 (Fig. 3). Importantly for long-term therapeutic potential, after multiple generations, S. aureus never developed resistance to the antimicrobial effects of lugdunin or escaped the degradation induced by Esp. This lack of resistance is in sharp contrast to traditional antibiotics against which organisms evolve resistance and emphasizes that naturally derived products may be a more effective means to inhibit opportunistic pathogens.
In a separate study, multiple coagulase-negative Staphylococcus spp., S. epidermidis and S. hominis were shown to produce novel lantibiotics that were able to synergize with the human cathelicidin antimicrobial peptide LL-37 and to inhibit the growth of S. aureus60. Strains producing these lantibiotics were depleted in individuals with atopic dermatitis, who are frequently colonized with S. aureus. In addition, the topical application of these antimicrobial-producing strains decreased the colonization of S. aureus in a small number of individuals with atopic dermatitis, demonstrating the translational potential of a probiotic strategy60.
Notably, not all microorganisms inhibit S. aureus; rather, it was found that some Propionibacterium species could induce S. aureus aggregation and biofilm formation in a manner dependent on dose, growth phase and pH61 (Fig. 3). In a separate in vitro study, S. aureus was found to change from virulent to commensal when exposed to the commensal Corynebacterium striatum62. This ability to alter S. aureus behaviour opens the therapeutic option of modulating their behaviour rather than destroying the pathogen62.
Examples of interactions between other skin microorganisms also exist. Corynebacterium accolens modifies the local environment of the skin to inhibit growth of the opportunistic pathogen Streptococcus pneumoniae63. This response was dependent on C. accolens using the lipase activity of LipS1 to release antibacterial free fatty acids from skin surface triacylglycerols. In another study, pairwise antagonism assays were performed with isolates from culture collections of S. epidermidis and P. acnes64. One P. acnes clade I-2 exhibited selectively higher antimicrobial activity against S. epidermidis than other P. acnes clades, likely owing to a thiopeptide conserved across type I-2 strains. Conversely, the majority of S. epidermidis strains tested were capable of inhibiting P. acnes growth in vitro. The authors of this study computationally predicted a variety of different mobile genetic elements that could be responsible for this phenotype in different strains. In a broader study of 89 isolates from six Staphylococcus spp., 84% of the isolates could produce antimicrobial molecules that target common skin bacteria65, indicating that bacteriocin capacity is an evolutionary conserved trait among skin commensals.
In contrast to many inter-species interaction studies, investigations of the dynamics between strains within a species are rarer. Extrapolations from metagenomic data have revealed two patterns of strain colonization of the human infant gut. For some species, there is a single dominant strain, whereas for other species, multiple strains coexist at similar levels66.
In the skin, P. acnes and S. epidermidis exist as stable heterogeneous communities of strains23,25. Pan-genome analyses of P. acnes suggested that functional saturation, or containing the entire gene encoding potential found in the pan-genome of this species, drives the maintenance and acquisition of multiple bacterial strains25. Within the gut, studies have shown that a community of Clostridium species can act synergistically to enhance regulatory T cell responses to a greater extent than any individual species could alone67. In the skin, similar studies are needed to demonstrate the possible functional advantages of heterogeneous strain communities.
The skin microbiome in disease
Interactions between members of the microbiota both shape the resident microbial community and prevent colonization by pathogenic bacteria in a process termed ‘colonization resistance’ (Ref. 68). However, in certain contexts, bacteria that are ordinarily beneficial to their hosts can become pathogenic. Many common skin diseases are associated with changes in the microbiota, termed dysbiosis69. This dysbiosis is often driven by common commensal species, as described below for acne, eczema and chronic wounds. Both rare and common skin disorders are thought to have underlying contributions both from individual species and from alterations to the microbial community. Additional longitudinal clinical studies may elucidate a mechanistic link between fungal species and dandruff or toenail infections and between viruses and warts.
Microorganisms associated with common acne. The prevalent teenage condition acne vulgaris is a chronic inflammatory skin condition that is associated with the bacterium P. acnes70, the most abundant organism in the microbiota of healthy adults18,71. At a functional level, gene expression profiles of P. acnes are distinct between individuals with acne and individuals without acne72. The observation that almost all adults are colonized with P. acnes but only a minority have acne highlights the importance of studying diseases in the broader context of host genetics, immune or barrier defects, the microbiome and the environment. For example, increased sebum secretion is associated with the pathophysiology of acne, as secretion rates correlate with the severity of clinical symptoms73. In a study using fluorescent microscopy to visualize P. acnes in follicles of skin biopsy samples, acne development was substantially associated with the presence of P. acnes in follicles and its formation of biofilms74. At the clade level, P. acnes belonging to the type 1A1 phylogroup have been consistently associated with acne across studies utilizing distinct sampling and analysis methods71,75,76,77. Strains within the type 1A1 phylogroup have increased inflammatory potential based on the presence of putative virulence factors that affect bacterial adhesion and host immune responses78.
Historically, vitamin B12 supplementation has been associated with acne in a subset of individuals79,80,81,82,83. Recently, this has been linked to supplemental vitamin B12 repressing vitamin B12 biosynthesis in P. acnes, which subsequently increases the production of porphyrins that can induce skin inflammation and acne development72. Interestingly, acne-associated P. acnes strains were found to produce substantially higher levels of porphyrins84.
Staphylococcus aureus and atopic dermatitis. Atopic dermatitis (also known as eczema) is a chronic, relapsing inflammatory disease with multiple contributing factors, including epidermal barrier impairment, immune cell activation and alterations in the community of associated skin microorganisms. Atopic dermatitis susceptibility has been associated with mutations in over 30 host gene loci, including the gene encoding skin barrier protein filaggrin85 and genes linked to the immune system86. In addition to S. aureus, which is commonly cultured from the skin of individuals with atopic dermatitis87, there are additional factors that support the hypothesis that microbiota have an influential role in disease pathogenesis. Atopic dermatitis is clinically treated with emollients that promote barrier integrity and immunosuppressive medications, such as steroids88. In cases where there is an infection or disease persistence, antimicrobial approaches (for example, antibiotics and dilute bleach baths) may be used, and their success has been shown to correlate with decreases in the relative abundance of S. aureus4; however, their overall effectiveness is uncertain89. As described above, much research is aimed to develop novel therapies specific to anti-S. aureus to replace the more broad-spectrum antimicrobials that are currently used.
In longitudinal studies of paediatric individuals with atopic dermatitis, 16S rRNA and whole genome sequencing of clinical samples showed that the relative abundance of Staphylococcus spp., particularly S. aureus and S. epidermidis, increased in the flare (episodic exacerbation) versus the post-flare state and that the relative abundance of staphylococci correlated with more severe disease at flare4,90. At the strain level, individuals with atopic dermatitis were found to be colonized with heterogeneous communities of S. epidermidis, and those with more severe disease were colonized with dominant S. aureus strains90. The correlation of S. aureus with atopic dermatitis during active disease exacerbation is well documented. However, the functional role of staphylococci in driving the atopic dermatitis disease state is poorly understood. Longitudinal sampling at more frequent intervals before a flare is still needed to identify whether increased staphylococci levels precede clinical symptoms, which would support the notion that staphylococci contribute to the initial onset of inflammation rather than bloom as a consequence of it. This warrants further investigation, as preliminary studies found a greater abundance of Staphylococcus spp. at 2 months in infants who did not develop atopic dermatitis by age 1 than in those who did develop atopic dermatitis by age 1. This suggests that Staphylococcus spp. exposure at an early age is helpful for proper education of the immune system91.
Another genome sequencing study compared the unaffected skin of adults with atopic dermatitis with that of a control cohort and identified an enrichment of Streptococcus spp. and Gemella spp. and a depletion of Dermacoccus spp. in individuals prone to atopic dermatitis92. At a functional level, the study showed that the microbiome of these individuals is primed to generate excess ammonia, providing an explanation for the high pH levels that are observed during atopic dermatitis flares92.
The decreased diversity of the skin microbiome in individuals with atopic dermatitis has been linked to a reduction in environmental biodiversity in the areas surrounding their homes93. In one study, healthy individuals had greater diversity of gammaproteobacteria in their skin, the presence of which correlated with greater IL-10 expression in blood93. A follow-up study using in vitro and in vivo animal experiments showed that the gammaproteobacteria genus Acinetobacter could induce strong T helper 1 (TH1) and anti-inflammatory immune responses that were protective against allergic inflammation94. In a study that examined the microbiome of unaffected skin of individuals with ichthyosis vulgaris and a filaggrin deficiency, there was an under-representation of Gram-positive anaerobic cocci compared with their presence in healthy controls, indicating that a defective stratum corneum is sufficient to alter the skin microbiome and may drive the dysbiosis that is associated with eczema95.
Owing to the association of S. aureus with atopic dermatitis, other skin diseases and bloodstream infections, many studies have focused on interactions between S. aureus, its toxins and the immune system. For example, S. aureus δ-toxin induces the degranulation of mast cells, which promotes both innate and adaptive type two immune responses96. S. aureus α-toxin can also induce IL-1β production from monocytes, which may consequently promote a TH17 response, or from CD4+ T cells making the cytokine IL-17 (Ref. 97). By contrast, when exposed to S. aureus-derived cell wall component lipoteichoic acid, T cells neither proliferated nor produced cytokines98, indicating that S. aureus products can activate the immune system and also temporarily paralyse it. In addition to targeting immune cells, S. aureus has also been shown to trigger adipocytes to rapidly proliferate and to produce increased levels of the antimicrobial peptide cathelicidin as a host defence mechanism99. These examples demonstrate the many ways that S. aureus could initiate or exacerbate skin disorders in the broader context of barrier defects or altered immunity. In fact, it has been demonstrated that in the context of barrier defects, S. aureus is able to traverse the epidermis into the dermis, where it encounters immune cells and triggers the expression of the inflammatory cytokines IL-4, IL-13 and IL-22 and thymic stromal lymphopoietin100. Notably, the ability of S. aureus to trigger the cutaneous immune response can be strain-dependent90, highlighting the importance of evaluating a phenotype across isolates of a species. Although many of these experiments were performed in murine models, they are relevant to humans, as many of the pathways underlying inflammation and immunity in murine skin appear relevant in human infection and disease. Additional examples of interactions between skin microorganisms and immune cells are discussed in Box 2.
Although the inflammatory potential of S. aureus has been demonstrated and dysbiosis is common to many skin diseases, it is still unknown whether these changes are a consequence of the disease state or whether S. aureus contributes to the initiation of the disease. Experiments with mouse models that are genetically and physically challenged to produce skin barrier or immunological defects have been used to determine the contribution of the microbiota to skin disease. For example, mice deficient in disintegrin and metalloproteinase domain-containing protein 17 (ADAM17) developed eczematous dermatitis as a consequence of microbial dysbiosis101. Alterations in cutaneous microbial communities, characterized by an overgrowth of Corynebacterium mastitidis, Corynebacterium bovis and S. aureus, preceded the development of features of atopic dermatitis. Targeted antibiotic treatment of these animals was sufficient to reverse the dysbiosis and eliminate skin inflammation, thus demonstrating a causal link between skin barrier alterations, dermatitis and the microbiome.
Skin microbiome of individuals with primary immunodeficiency. While several studies have investigated how microorganisms educate the immune system, the study of individuals with primary immunodeficiency (PID) provides an opportunity to understand the role of immunity in determining the structure of microbial communities. Underlying the rationale for these investigations are the common cutaneous manifestations of individuals with PID, particularly the eczematous features. To study this, skin microbiota samples were taken from individuals with rare monogenic PIDs, hyper immunoglobulin E (IgE) syndrome, Wiskott–Aldrich syndrome and dedicator of cytokinesis 8 syndrome. Despite distinct underlying mutations, all diseases are characterized by eczematous-like skin disease, reduced T and B cells, variable eosinophilia and elevated IgE levels102. Although overall similar in the types of bacteria that colonize the skin of healthy individuals, the skin of individuals with PID is more ecologically permissive with decreased temporal stability102. Despite individuals with PID being colonized with opportunistic fungi (for example, Candida spp. and Aspergillus spp.) and bacteria (for example, Serratia marcescens), which are typically absent in controls, these microorganisms still belong to phyla that are commonly associated with the skin. This suggests that organisms outside of these primary phyla are unable to stably survive in the nutrient-poor environments of the skin. In a separate study of individuals with PID caused by mutations in signal transducer and activator of transcription 1 (STAT1) or STAT3, the skin was colonized with more Gram-negative bacteria, particularly Acinetobacter spp., and there was a reduction in Corynebacterium spp. colonization compared with the levels in healthy controls103. To identify possible alterations in the viral communities, shotgun metagenomic sequencing of samples from these individuals is needed; these studies are clinically relevant, as some individuals with PID commonly suffer from viral skin infections104.
Microorganisms in chronic wound infections. In addition to classical skin diseases, microorganisms that colonize the skin have also been shown to affect the healing of chronic wounds prevalent in populations that are elderly or have diabetes or obesity. For example, the role of microorganisms has been well studied in the case of diabetic foot ulcers (DFUs). It is estimated that over 50% of DFUs are infected105. DFUs are a common result of diabetes-induced neuropathy and will occur in 15–25% of individuals with diabetes106, with 15.6% requiring amputation107. A 16S rRNA sequencing survey found that bacterial communities colonizing neuropathic DFUs were associated with clinical features108. For example, shallow ulcers and those of short duration were associated with greater abundances of Staphylococcus spp., particularly S. aureus, whereas deeper ulcers and those of longer duration had greater microbial diversity and a higher relative abundance of anaerobic bacteria and Gram-negative Proteobacteria spp.108. In addition, poor control of blood glucose was associated with greater Staphylococcus spp. and Streptococcus spp. colonization108.
In a longitudinal survey of microorganisms associated with DFUs, 16S rRNA sequencing of the wound revealed that bacterial community instability was associated with faster healing and more positive clinical outcomes109. This observation is counterintuitive, as many studies of other body sites have associated disease with bacterial community instability4,110. However, in the context of a wound, microbial instability could result in effective clearance of wound bacteria by the immune system. In addition to bacteria, the fungal community was also explored in the same cohort with amplicon sequencing of the ITS1 region111. Fungi were identified in 80% of the 100 DFUs analysed, with Cladosporium herbarum and Candida albicans identified as the most abundant species. In chronic wounds with poor clinical outcomes fungal diversity was increased and polymicrobial biofilms of fungi and bacteria were commonly found111.
Conclusions and outlook
In summary, this Review provides an analysis of the skin microbiome in health and disease at previously unexplored resolution. Analysis at this level was possible owing to technical advances in DNA extraction techniques and sequence library preparation methods that have been optimized for the diverse yet low biomass of skin samples. Moreover, the development of novel software pipelines that exploit the depth of information that is available in shotgun metagenomic sequencing data has advanced our understanding of the human skin microbiome. However, many questions remain regarding the function of the skin microbiota: what role do microorganisms have in the skin in maintaining health or promoting disease states?
DNA sequencing is a useful and unbiased tool for revealing the microorganisms in a sample; however, it is unable to differentiate between live colonizing and dead transient organisms. Although traditional culture techniques can distinguish between live and dead microorganisms, results are skewed by the culture conditions used. RNA sequencing may address this issue by revealing the functional activity of the microbiota, but it is technically difficult given the low biomass of organisms on skin. To measure this activity indirectly, a new analysis technique was developed that compares read distributions at the origin of replication and with those elsewhere in the genome as evidence of active bacterial replication112.
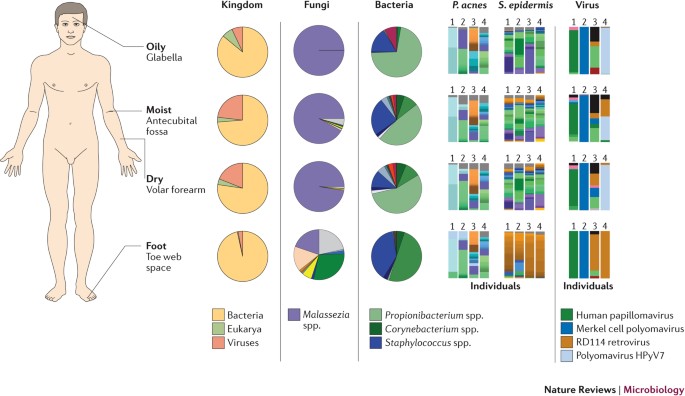
Analyses of microbiome sequencing data from patients compared with healthy controls can be used to generate hypotheses about putative disease-causing microorganisms (Fig. 4). Organisms of interest can then be isolated from individuals through targeted culturing methods. Next, these organisms can undergo whole genome sequencing to analyse their functional potential and can be tested in animal models to determine potential mechanistic roles in disease progression. Overall, the objective is to translate microbiome sequence data to functional studies that could inform the development of therapeutic modalities to ameliorate dysbiosis and counteract pathogens.
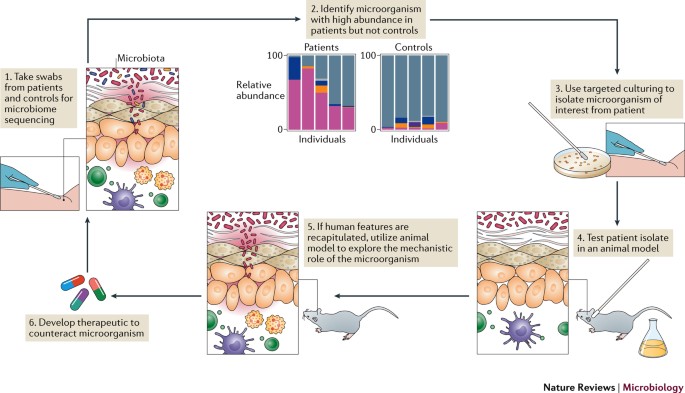
To begin, skin swabs are taken from healthy controls and patients at sites relevant to the disease of interest (step 1). For example, the bend of the elbow and back of the knee would be relevant for atopic dermatitis. These skin samples are sequenced, and microbial communities between patients and controls are compared (step 2). Differences between groups can be used to generate hypotheses around microbial drivers of the disease. To experimentally test the hypotheses from computational analyses, isolates of interest should be cultured from patients (step 3). Targeted culture conditions can be used to more easily cultivate the isolate of interest. The patient-derived isolates should then be tested in preclinical models relevant to the disease (step 4). If the microorganism is sufficient to recapitulate features of the human disease, additional experiments should be utilized to explore the mechanism of action of the microorganism (step 5). On the basis of results from the previous steps, a therapeutic should be developed to counteract pathogenic microorganisms (step 6). A similar model could also be utilized to identify and evaluate protective, beneficial microorganisms present in controls but absent or under-represented in patients.
[“source=nature”]