- Dermatologic Manifestations of Metastatic Carcinomas
- Cell Biology of Head and Neck Squamous Cell Carcinoma
- Metastatic Cancer With Unknown Primary Site
What drugs will oncologists be using in 2020? What classes of anti-cancer therapies will come after immunotherapy?
According to speakers at the 2016 European Society for Medical Oncology (ESMO) Congress, bacteria, viruses, and RNA therapeutics are just a few of the avenues being pursued as the next wave of new anti-cancer agents.
History of Bacteria and Viruses in Cancer Therapy
At ESMO, Ramon Alemany, PhD, a researcher at the Catalan Institute of Oncology in Barcelona, Spain, outlined why bacteria and viruses have great promise as anti-cancer agents: They are self-amplifying and can be tumor-selective, immunostimulatory oncolytic agents.
The idea of using bacteria and viruses as anti-cancer agents is not new, however. In 1290, clinicians documented a spontaneous regression of a leg tumor after an infection, and in 1890, William Coley injected Streptococcus pyogenes in 10 cancer patients, producing one complete response.[1] Over the next 40 years, injections of Coley’s toxins improved outcomes for over 1000 patients with bone and soft-tissue sarcomas.[1]
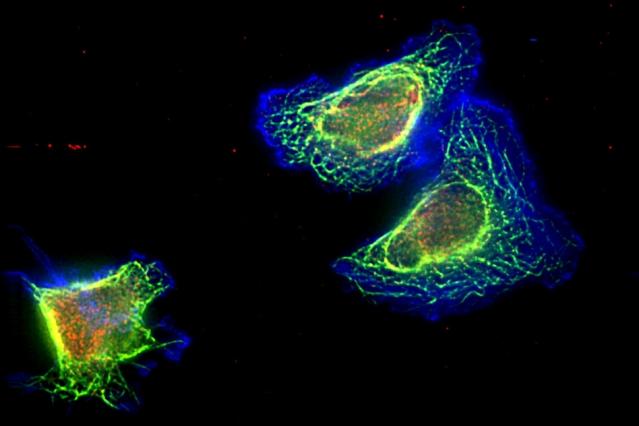
In the 1950s, scientists began testing interferon-sensitive viruses with natural oncotropism; interferon-sensitive viruses are still under development today.[2] Since the 1990s, scientists have been modifying viruses and bacteria to develop tumor selectivity. They are attenuated, so they replicate only in tumors cells, not normal cells. Scientists can reprogram viruses into oncolytic vectors by combining three types of modification: targeting, arming, and shielding.[3] Targeting introduces multiple layers of cancer specificity and improves safety and efficacy; arming occurs through the expression of prodrug convertases and cytokines; and coating with polymers followed by the use of different envelopes or capsids provides shielding from the host immune response.[3]
Research Trials and Clinical Use
The first oncolytic virotherapy approved on a widespread basis was talimogene laherparepvec (T-VEC), to treat surgically unresectable skin and lymph node lesions in patients with advanced melanoma.[4] The genetically modified virus produces granulocyte-macrophage colony-stimulating factor (GM-CSF). In the phase 3 OPTiM trial of patients with stage IIIB/C-IV M1a melanoma, the T-VEC arm experienced improved survival by a median of 20.4 months compared with those who received standard treatment with GM-CSF.[4] The response rate was 33% for the injected tumors, 16% for skin metastases, and 3% for visceral metastases. Also approved, but only in Latvia and Georgia, is Rigvir®, which contains a live nonpathogenic enteric cytopathic human orphan 7 virus that has not been genetically modified.[5] Rigvir is approved for melanoma and is used for several other solid tumor cancers, including pancreatic cancer, kidney cancer, and lung cancer.
Some of the challenges of virotherapy, said Dr Alemany, include systemic delivery, intratumoral spread, and improving anti-tumor versus anti-virus immune response. One way of improving virotherapy is to mask the virus from neutralizing antibodies using albumin.[6] Another strategy is to arm viruses with hyaluronidase, an enzyme that catalyzes the hydrolysis of hyaluronic acid. The main source of physical resistance to drug transport is the presence of high amounts of extracellular matrix (ECM) and high interstitial fluid pressure in tumor interstitium; hyaluronan is an important structural element of the ECM.[7] Arming viruses with hyaluronidase allows cancer drugs to reach malignant cells. Continue Reading
[“source-smallbiztrends”]

 Prize Honors Innovations to Improve Cancer Patient Experience
Prize Honors Innovations to Improve Cancer Patient Experience Clinical Takeaways From the ESMO Presidential Symposia
Clinical Takeaways From the ESMO Presidential Symposia